When I was a teenager I wasn’t focused on much, especially the value a good education could bring to my life. I really couldn’t see past what was happening at the weekend. It’s not an excuse but Ireland was a pretty bleak place to grow up, and I grew up in a household where there was little encouragement to do well academically. It also didn’t help that I had absolutely no idea what I would like to do so I drifted along after school from job to job with no focus just an underlying feeling of frustration that things somehow weren’t better.
When I got my stage 4 diagnosis it was very much the kick up the arse to focus me. I knew a little about melanoma as I had been diagnosed stage 2 just over ten years earlier. But this was different my life was now in immediate danger. Once I had regained some strength and went from hopelessness to a small sliver I set about learning what I could to help myself and by default other patients. This has somehow snowballed beyond any expectation I set out with.
I decided early on that I was going to follow Jim Carey’s mantra in” YES Man”. If there was an opportunity I would go for it. As I put myself out there my network of useful connections began to grow rapidly. Patients often complain that they don’t get enough information, but at the same time can’t specify what exactly it is they want. I know sometimes that information they seek is the easy miracle cure, that will take away all their health problems, understandable if not realistic.
I am a bit more pragmatic. For me that miracle cure is sort of and elusive dream although I continue to do well on my current treatment (at least I hope I am scans again shortly, will tell). What I could do though was engage and learn so that I give myself the very best chance by understanding the treatments and the system that provides them.
As I stumbled around sometimes literally at international conferences, it became very clear to me that there was a real need for the patients voice to be represented, but I felt silly and uncomfortable calling myself a patient advocate. I didn’t believe I had earned it, I certainly didn’t feel I understood enough, even though I was never afraid to stick my hand up and ask an awkward question. I became aware of the EUPATI patient education program but I wasn’t comfortable committing to eighteen months of study, I wasn’t sure I’d get to the end and it seemed unfair to take a much sought after place on that course that could benefit some other patient representative. Maybe it was a little pessimistic on my part but it was how I was feeling when the application process opened, so I decided to “Let it Go”.
Around the corner, a new opportunity arose from one of my connections. IPPOSI ( Irish Platform for Patient Organisations Science & Industry) had developed a course based on that european Eupati model but with an Irish slant. It was shorter, focused on Irish systems, and I could clearly see how it would be beneficial to an Irish patient advocate. I didn’t have to think twice about applying.

The course began in September 2017 with a module on understanding Clinical Trials. Prof Peter Doran of UCD School of Medicine made it very clear as an institution they aren’t in the business of dumbing down information. We were in at the deep end but it was ok I had my fellow students, the faculty at UCD and IPPOSI supporting us. We began six months course work that often demanded daily attention. There were face to face workshops, online tutorials and assignments coupled with the dreaded weekly knowledge quiz. Two more modules followed with the HPRA (Health Products Regulatory Authority) teaching us about the regulation of medicines from a safety perspective, the importance of patients reporting side effects to such regulatory authorities and the opportunities to engage at a european level with the European Medicines Agency as patient advisers.
Our final module began in January on the often controversial process of health technology assessment by our national HTA body the National Centre for Pharmacoeconomics (NCPE) They are often viewed by the public as the ones who don’t want to pay for patients to have a particular treatment, ending up with frustrated desperate patients protesting at the gates of Dáil Éireann. That’s a scenario patients don’t want to find themselves in, it’s hard enough being sick. There is a growing understanding from such decision-making bodies that engaging patients in the process learning from each other is a much more beneficial model of business for all concerned.
My fellow students have also been a real source of information and experience. Our chats over coffee and listening to their contributions during workshop discussions has been enlightening. We all came with different medical problems different expectations and agendas but we managed to gel together. They really made the course valuable as much as the lecturers. Opportunities to go forward and make a difference as patient representatives feel more tangible now we have graduated.
So somehow after spending years drifting, not knowing what it is I wanted to do when I grow up (something I’m still working on) I’ve by default found an area I’m really engaged and interested in, and amazingly a certificte from UCD school of Medicine on understanding Clinical Trials. Unfortunately it came about because of what’s classified as a life limiting illness, but Hey Ho!! When life gives you lemons go out and make lemonade……… 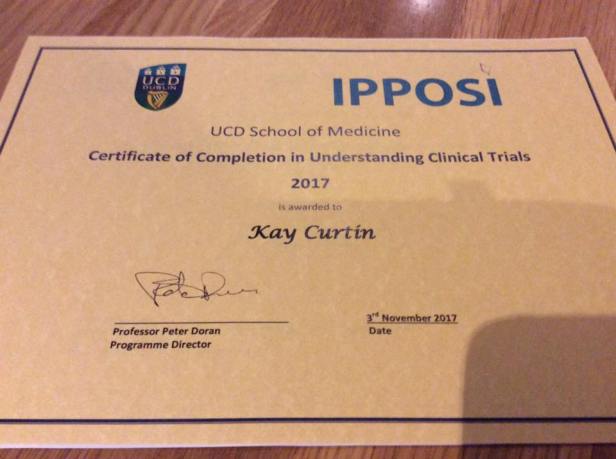

great piece of writing.. Well done a fantastic achievement. the world’s you oyster now.. best of luck..
LikeLiked by 1 person
As ever an inspiration and so so proud of you.X
LikeLiked by 1 person